Our website is made possible by displaying online advertisements to our visitors.
Please consider supporting us by disabling your ad blocker.
Idiopathic pulmonary fibrosis
| Idiopathic pulmonary fibrosis | |
|---|---|
| Other names | Fibrosing alveolitis, cryptogenic fibrosing alveolitis, diffuse fibrosing alveolitis, usual interstitial pneumonitis, diffuse interstitial pneumonitis |
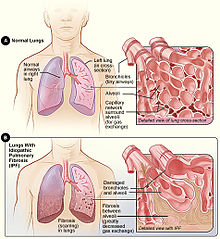 | |
| Figure A shows the location of the lungs and airways in the body. The inset image shows a detailed view of the lung's airways and air sacs in cross-section. Figure B shows fibrosis (scarring) in the lungs. The inset image shows a detailed view of the fibrosis and how it damages the airways and air sacs.[1] | |
| Specialty | Pulmonology |
| Symptoms | Shortness of breath, dry coughing[1] |
| Complications | Pulmonary hypertension, heart failure, pneumonia, pulmonary embolism[1] |
| Usual onset | Gradual[1] |
| Causes | Unknown[2] |
| Risk factors | Cigarette smoking, certain viral infections, family history[1] |
| Diagnostic method | CT scan, lung biopsy[3] |
| Differential diagnosis | Sarcoidosis, other interstitial lung diseases, hypersensitivity pneumonitis[4] |
| Treatment | Pulmonary rehabilitation, supplemental oxygen, lung transplantation[1] |
| Medication | Pirfenidone, nintedanib[2] |
| Prognosis | Life expectancy ~ 4 years[1] |
| Frequency | 12 per 100,000 people per year[4] |
Idiopathic pulmonary fibrosis (IPF) synonymous with cryptogenic fibrosing alveolitis[5] is a rare, progressive illness of the respiratory system, characterized by the thickening and stiffening of lung tissue, associated with the formation of scar tissue. It is a type of chronic pulmonary fibrosis characterized by a progressive and irreversible decline in lung function.[6][3][4]
The tissue in the lungs becomes thick and stiff, which affects the tissue that surrounds the air sacs in the lungs.[7] Symptoms typically include gradual onset of shortness of breath and a dry cough.[1] Other changes may include feeling tired, and clubbing abnormally large and dome shaped finger and toenails.[1] Complications may include pulmonary hypertension, heart failure, pneumonia or pulmonary embolism.[1]
The cause is unknown, hence the term idiopathic.[2] Risk factors include cigarette smoking, acid reflux disease (GERD), certain viral infections, and genetic predisposition.[1] The underlying mechanism involves scarring of the lungs.[1] Diagnosis requires ruling out other potential causes.[3] It may be supported by a high resolution CT scan or lung biopsy which show usual interstitial pneumonia.[3] It is a type of interstitial lung disease.[3]
People often benefit from pulmonary rehabilitation and supplemental oxygen.[1] Certain medications like pirfenidone (Esbriet) or nintedanib (Ofev) may slow the progression of the disease.[2] Lung transplantation may also be an option.[1]
About 5 million people are affected globally.[8] The disease newly occurs in about 12 per 100,000 people per year.[4] Those in their 60s and 70s are most commonly affected.[4] Males are affected more often than females.[4] Average life expectancy following diagnosis is about four years.[1] Updated international guidelines were published in 2022, which some simplification in diagnosis and the removal of antacids as a possible adjunct therapy.[9]
- ^ a b c d e f g h i j k l m n o "Idiopathic Pulmonary Fibrosis". NHLBI. Retrieved 21 January 2018.
- ^ a b c d Raghu G, Rochwerg B, Zhang Y, Garcia CA, Azuma A, Behr J, et al. (July 2015). "An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline: Treatment of Idiopathic Pulmonary Fibrosis. An Update of the 2011 Clinical Practice Guideline". American Journal of Respiratory and Critical Care Medicine. 192 (2): e3–19. doi:10.1164/rccm.201506-1063ST. PMID 26177183.
- ^ a b c d e Raghu G, Collard HR, Egan JJ, et al. (2011). "An official ATS/ERS/JRS/ALAT statement: Idiopathic pulmonary fibrosis: Evidence-based guidelines for diagnosis and management". American Journal of Respiratory and Critical Care Medicine. 183 (6): 788–824. doi:10.1164/rccm.2009-040GL. PMC 5450933. PMID 21471066.
- ^ a b c d e f Ferri FF (2017). Ferri's Clinical Advisor 2018 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 691. ISBN 9780323529570.
- ^ "Idiopathic pulmonary fibrosis | Information for the public | Idiopathic pulmonary fibrosis in adults: diagnosis and management | Guidance | NICE". www.nice.org.uk. 12 June 2013. Retrieved 15 June 2024.
- ^ Todd, Nevins W.; Luzina, Irina G.; Atamas, Sergei P. (2012). "Molecular and cellular mechanisms of pulmonary fibrosis". Fibrogenesis & Tissue Repair. 5 (1): 11. doi:10.1186/1755-1536-5-11. PMC 3443459. PMID 22824096.
- ^ "Idiopathic Pulmonary Fibrosis". NHLBI, NIH. Retrieved 5 December 2020.
- ^ Meltzer EB, Noble PW (2008). "Idiopathic pulmonary fibrosis". Orphanet Journal of Rare Diseases. 3 (1): 8. doi:10.1186/1750-1172-3-8. PMC 2330030. PMID 18366757.
- ^ Raghu, Ganesh; Remy-Jardin, Martine; Richeldi, Luca; Thomson, Carey C.; Inoue, Yoshikazu; Johkoh, Takeshi; Kreuter, Michael; Lynch, David A.; Maher, Toby M.; Martinez, Fernando J.; Molina-Molina, Maria; Myers, Jeffrey L.; Nicholson, Andrew G.; Ryerson, Christopher J.; Strek, Mary E. (1 May 2022). "Idiopathic Pulmonary Fibrosis (an Update) and Progressive Pulmonary Fibrosis in Adults: An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline". American Journal of Respiratory and Critical Care Medicine. 205 (9): e18–e47. doi:10.1164/rccm.202202-0399ST. ISSN 1073-449X. PMC 9851481. PMID 35486072. S2CID 248432749.
Previous Page Next Page
تليف رئوي مجهول السبب Arabic Идиопатична белодробна фиброза Bulgarian Fibrosi pulmonar idiopàtica Catalan Idiopathische Lungenfibrose German Ιδιοπαθής πνευμονική ίνωση Greek Fibrosis pulmonar idiopática Spanish فیبروز ریوی ایدیوپاتیک FA Idiopaattinen keuhkofibroosi Finnish Fibrose pulmonaire idiopathique French פיברוזיס ריאתי אידיופתי HE


